Why in the News?
The Prime Minister has reaffirmed the government’s dedication to addressing sickle cell disease, a genetic blood disorder that alters the shape of red blood cells.
What is SCD?
- Sickle cell disease, a chronic condition, encompasses a group of inherited disorders affecting haemoglobin, the protein responsible for oxygen transport in the body.
- Typically, red blood cells possess a disc-like shape and are flexible, facilitating smooth movement through blood vessels.
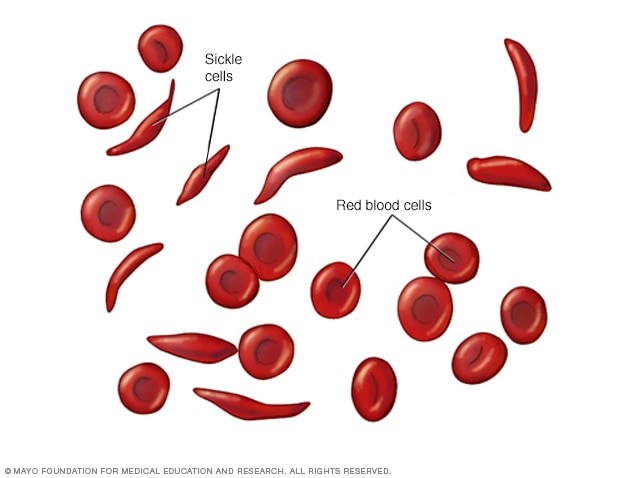
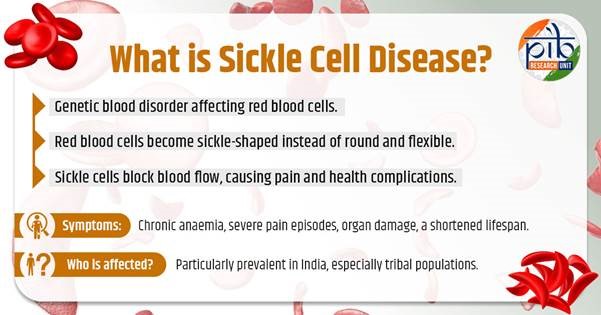
- However, in SCD, a genetic mutation causes these red blood cells to adopt a crescent or “sickle” shape.
- These sickle-shaped RBCs lead to disruption of blood flow in small vessels and result in numerous complications.
Understanding the burden
- SCD affects 20 million people worldwide. India grapples with a formidable challenge posed by SCD, with millions affected.
- According to an article by Forbes, India has the second-highest global prevalence of the disease, with one in 86 births positive for SCD.
- And-organ damage and increased infection susceptibility, Stroke and pulmonary complications,
Challenges: the challenges presented by SCD are diverse
- The geographic and socioeconomic disparities exacerbate the challenges faced by individuals living with SCD,
- Accessibility remains a formidable barrier impeding optimal care for individuals with SCD
- High Disease Burden: India has the world’s second-largest burden of sickle cell disease, with over a million affected individuals, primarily in tribal areas.
- Low Treatment Coverage: Only 18% of those affected receive consistent treatment, with significant drop-offs in screening, diagnosis, and treatment adherence.
- Stigma and Misinformation: Social stigma around the disease, myths such as “God’s curse” or “black magic,” and mistrust of public health systems, particularly in tribal areas, result in delayed diagnosis and treatment.
- Treatment Adherence Issues: Challenges include inconsistent availability of medicines like hydroxyurea, long travel distances for treatment, and stock shortages at health centres.
- Poor Vaccination Coverage: Vaccination, which reduces infection rates and improves quality of life, remains inadequate in many affected regions.
- Research and Development: The lack of ongoing research into treatments and understanding of the disease in India, and the unaffordability of emerging therapies like gene therapy, hinder long-term progress.
- Financial and Operational Gaps: Health systems in tribal areas require additional funding and operational strengthening to address region-specific health challenges effectively.
COMBATING SCD IN INDIA:
For combating SCD in India multifaceted approach is required:
- A holistic approach that encompasses early diagnosis, promoting early screening and intervention.
- Scientific innovation,( Advancing SCD research, enhancing patient care)
- fostering collaborations
- Robust healthcare infrastructure
- Community empowerment.
- The urgent need for targeted interventions (newborn screening and early diagnosis )
- Universal access to proven medications like hydroxyurea is crucial, emphasising the need for scalable solutions to ensure widespread availability.
- Collaborative initiatives: Collaborative efforts between healthcare stakeholders, government agencies, and pharmaceutical entities are imperative to streamline the distribution channels and bridge existing gaps in accessibility
- Fostering partnerships with community
- Community-driven initiative aimed at raising awareness about SCD among tribal communities in rural India
- Empowering tribal communities holds the key to addressing the endemicity of SCD in India.
- Community engagement, culturally sensitive interventions, and capacity-building initiatives are essential to effect meaningful change.
- By leveraging indigenous knowledge systems, fostering partnerships with community leaders, and prioritising grassroots healthcare infrastructure, can engender sustainable solutions tailored to the unique needs of tribal populations.
- Awareness drives: Through interactive workshops, educational campaigns, and storytelling sessions, the initiative succeeded in dispelling myths surrounding SCD
- Research and collaboration
- Research and collaboration Sustained investment in translational research and clinical trials is needed to realise the promise of gene therapy and other emerging treatments.
- Additionally, initiatives aimed at understanding genetic modifiers and environmental factors influencing SCD manifestation hold immense potential in refining treatment strategies and improving patient outcomes.
- Digital health technologies
- The advent of precision medicine and digital health technologies presents unprecedented opportunities in SCD management.
- Telemedicine, wearable devices, and remote monitoring solutions can enhance patient care, particularly in underserved regions.
- Advances in artificial intelligence and machine learning hold promise in predicting disease complications, optimising treatment regimens, and personalising therapeutic approaches based on individual patient profiles.
- Global collaboration
- Global collaboration is essential in addressing the multifaceted challenges posed by SCD.
- Forging partnerships with international organisations, academic institutions, and philanthropic foundations can accelerate progress in SCD research and advocacy.
- Collaborative initiatives aimed at harmonising treatment guidelines, and sharing best practices can amplify the impact of individual efforts and drive meaningful change on a global scale.
- Policy advocacy
- It plays a pivotal role in shaping the healthcare landscape and addressing systemic barriers to SCD care.
- Policy reforms aimed at prioritising SCD screening, prevention programmes improving access to essential medications, and strengthening of healthcare infrastructure, are needed.
- Engaging policymakers and advocating for legislative changes can catalyse transformative reforms that prioritise the needs of individuals living with SCD and ensure equitable access to quality care.
What are the WHO recommendations?
- Early Identification: Implement newborn screening programs to identify sickle cell disease at birth.
- Integration into Health Systems: Sickle cell management should be integrated into national health services.
- This includes establishing specialized centres for comprehensive care and ensuring that primary healthcare providers are trained in managing sickle cell disease.
- Public Education and Awareness: Conduct public education campaigns to raise awareness about sickle cell disease, reduce stigma, and inform communities about genetic risks and prevention strategies.
- Genetic Counselling: Provide genetic counselling to families, especially in communities with high prevalence, to inform them about the risks of having children with sickle cell disease and the importance of carrier screening.
The National Sickle Cell Anaemia Elimination Mission
- The Indian government initiated the National Sickle Cell Anaemia Elimination Mission in 2023, aiming to eradicate SCD by 2047.
- This initiative entails enhancing awareness, conducting universal screening of approximately seven crore individuals aged 0-40 in affected tribal regions, and providing counselling through collaborative endeavours between central ministries and State governments
- The mission aims to reduce the burden of sickle cell disease, which primarily affects India’s tribal belt (Odisha, Jharkhand, Chhattisgarh, Madhya Pradesh, Maharashtra).
- These include nationwide screening programs and the inclusion of vital medicines like hydroxyurea in the essential medicines list, improving access to treatment
Source: the Hindu & PIB

 MPSC राज्य सेवा – 2025
MPSC राज्य सेवा – 2025
